Home > COVID-19: The Challenges for People living with Dementia
By Shivani Patel and Jiabin Tang


To download this article as a pdf please click here.
Introduction
Recently, all our lives have been turned upside-down by the Coronavirus (COVID-19) pandemic. In this article we will describe the impact of the pandemic and the resultant ‘lockdown’ on people living with Lewy body dementia, and how the COVID-19 pandemic has changed the way we provide care.
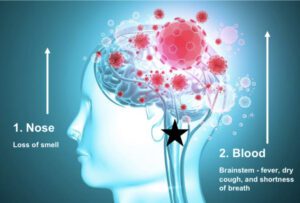
The main symptoms of COVID-19 are a high fever, a continuous cough, and a loss or change to your sense of smell or taste. Risk factors identified during the pandemic include: gender (male), age (≥60 years), where you live (higher risk in poorer areas), ethnic minority background (Black, Asian), being born outside UK and Ireland, living in a care home, certain jobs (nurses, taxi driver, security guard etc), and underlying health conditions (asthma, diabetes, heart disease etc) 3. According to the National Health Service (NHS), people with diseases affecting the brain or nerves are at moderate risk of catching the virus as they are ‘clinically vulnerable.’
COVID-19 in People with Dementia and Related Disorders
Vulnerability, age, and the co-occurrence of one or more conditions may mean that people with dementia and related disorders such as Parkinson’s Disease (PD) and Alzheimer’s Disease (AD) are at greater risk of COVID-19.
Dementia, a ‘pandemic’ itself in the ageing population, affects 50 million people worldwide with one new case emerging every 3 seconds 16. People living with dementia and related disorders may be particularly vulnerable to contracting COVID-19.
People living with these diseases may also find it harder to follow government guidelines designed to prevent the spread of the virus such as washing hands, covering one’s mouth or nose when coughing or sneezing, monitoring COVID-19 symptoms, maintaining the recommended physical distance and staying at home 17. People with mild cognitive impairment (MCI) or milder dementias may be unwilling to comply, simply due to their lack of interest (apathy) or depression. People with more severe dementia may not be able to understand or remember the guidelines due to their short-term memory loss and cognitive impairment 17.
Patients with advanced PD may be particularly vulnerable to COVID-19, due to rigidity of respiratory muscles, impairment of cough reflex and pre-existing difficulties in breathing (dyspnea) 18. Recent studies on patients with PD and COVID-19 have shown that older people with PD (mean age 78.3 years) with longer disease duration (mean 12.7 years) are more susceptible to COVID-19 than those without PD 18. People on advanced therapies, such as deep brain stimulation (DBS) or levodopa infusion therapy, are even more vulnerable. However, responses may also vary between countries based on pandemic severity and lockdown duration.
COVID-19 VS Chronic Brain Diseases – Dilemmas in Management
Neurological care has been compromised due to the pandemic and strain on health care systems 19. Healthcare systems have been forced to divert medical care due to the COVID-19 pandemic, dramatically impacting patients with chronic conditions such as dementia. Appointments have been postponed, surgical procedures delayed, and some people have also decided to skip or postpone appointments due to the risk of being exposed to the virus 20.
Furthermore, lockdown, self-isolation and social distancing have raised concerns of wellbeing for people with chronic illnesses 21,22. Lockdown restricts access to healthcare and physical exercise 22, increasing psychological stress and anxiety as well as consequences of prolonged immobility. Self-isolation and social distancing can be detrimental for mental health. Generally, people with dementia tend to experience increased depression, anxiety, irritability, and general restlessness 23,24, and these symptoms are likely to become more severe with quarantine. Lack of physical activity could worsen motor and non-motor symptoms, such as insomnia (inability to sleep), and constipation (difficulty in emptying bowels).
Nonetheless, new support initiatives are available. The pandemic has stimulated the use of telemedicine to deliver urgent and ongoing healthcare 21,25. Telemedicine means the use of electronic information and communication technology to support healthcare when physical distancing measures apply. Online solutions are available to reduce the feeling of social isolation and for providing a sense of comfort and hope. This includes video-conferencing, smartphone health care applications, simple telephone communication, email and text messages 26,27. Video-conferencing, or online consultation, is a strategy that enables doctors to remain connected and monitor patient health without face-to-face contact 28,29. Educational media, such as webinars and informative websites, have also been implemented for health care providers and patients. Remote strategies to promote well-being such as online exercise classes and home-based exercises for patients should also be promoted 30, as well as mental health care through guidance on reducing stress, relaxation and meditation exercises 16.
Conclusion
The COVID-19 pandemic has disrupted the entire world in unprecedented ways. Nevertheless, scientists are augmenting their research by studying the effect of COVID-19 on people living with dementia, potentially opening up more avenues for treatment in future. New remote medicine methods and systems used in the crisis can be further developed and maintained in future to improve patient care and management. We know it has been difficult to stay at home but remember, we are all in this together and will come out stronger than ever.
References
To receive regular news updates, resources, events and breakthroughs in the fight against Lewy body dementia please enter your email address….
We will only contact you in relation to latest news & updates that we think will be of interest to you. We will not disclose your information to any third party and you can unsubscribe from our database at any time.
© 2023 The Lewy body Society. Registered Charity No: 1114579 (England and Wales) and SC047044 (Scotland). Website by ATTAIN